Quality Improvement Program
SNHN has a strong commitment to quality improvement in primary care; we provide free licences to all general practices in our region for data extraction and population management software, and ongoing support, which includes training and guidance for practices to effectively analyse their data and support for quality improvement activities.
Using a data extraction tool allows a practice to analyse its own data and enables the building and maintenance of disease registers, ensures you are meeting RACGP accreditation standards, facilitates data cleansing in practice software and participation in PIP QI. Clean data also facilitates the quality of information being shared with My Health Record
Practice staff will better understand the demographics and risk stratification of the patients attending the practice. Understanding the practice patient population is essential to improving patient care and outcomes and maximising practice return on investment by ensuring MBS item numbers are claimed correctly for the care provided.
SNHN provides support for all practices to embed Quality Improvement (QI) strategies in their day-to-day workflow. The Primary Care Advancement Team (PCAT) can help with the analysis of your data and identify areas for QI. An important aspect of quality improvement is goal setting and activities associated with each goal. We provide practices with quarterly data quality reports, which assist in guiding the direction of your QI activities.
Practice Incentives Program Quality Improvement (PIP QI)
Since the introduction of the PIP QI in August 2019, we continue to provide support to practices to achieve the required component of at least one quality improvement activity for each PIP QI quarter.
We now provide an additional separate report for the PIP QI Eligible Data Set of Measures to practices registered for PIP QI, to further assist driving QI initiatives.
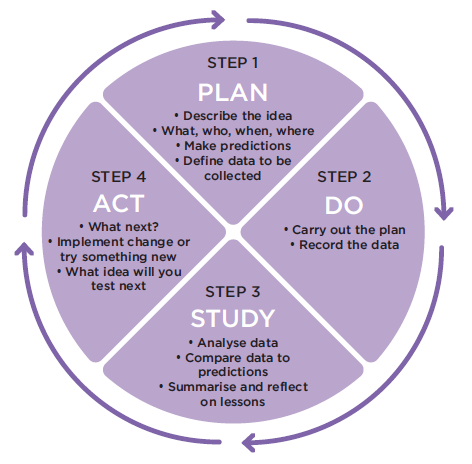
Quality Improvement needs to be approached in small steps, and we will offer assistances to do this by guiding practices in the Model for Improvement (MFI). The MFI consists of completing Plan, Do, Study, Act or PDSA cycles.
Engaging in quality improvement activities is an opportunity for the practices’ GPs and other staff members to collaborate as a team to consider quality improvement formalise, document and be remunerated (via PIP QI) and satisfies accreditation.
Not every change is an improvement, but by making small changes you can test ideas on a smaller scale before implementing bigger changes to meet the desired goal/s.
Free Data Extraction Software license
To support quality improvement in General Practice, and the Practice Incentives Program Quality Improvement (PIP QI), Sydney North Health Network (SNHN) offers practices in the region a free licence for a population health management and clinical audit tool for extracting, analysing, and managing deidentified general practice data in a confidential and safe way to general practices.
Some of the benefits to having a data extraction tool include efficient management of your patient population and practice staff can easily identify and target populations for review and management in areas such as chronic disease management, cancer screening, older persons’ care and mental health.
If you do not have a Data Extraction Tool installed and would like to participate in PIP QI, we can arrange this and guide you with the PIP QI requirements. Contact us at pcait@snhn.org.au
Primary Sense
A Primary Health Network initiative
Primary Sense is a Primary Health Network (PHN) owned and operated population health management, clinical decision support and data extraction tool.
Designed by GPs, data experts and researchers, Primary Sense extracts de-identified general practice data and uses evidence-based algorithms to provide GPs with real-time medication alerts, reports, and patient care prompts. It also provides general practices and Primary Health Networks (PHNs) with on-demand reporting to help with population health management.
Sydney North Health Network (SNHN) offers practices in the region a free license and installation for Primary Sense. We provide ongoing support, including training and guidance to practices for installing and using Primary Sense.
Data security
Primary Sense uses the highest standards of data security to extract, analyse and manage de-identified general practice data.
All data transmission is encrypted and sent over secure channels. It is stored or contained in reports that are locked down under multiple layers of access control. Data is governed responsibly, privacy protected and securely stored and managed in Australia by the PHN-owned Primary Health Insights (PHI) hosting platform. The platform features multiple layers of security and a comprehensive governance framework. It complies with Australian Privacy Principles and legislation.
To find out more about Primary Sense, please click here
Registration and Onboarding
- Data Sharing agreement
- Practice Registration Checklist form
- Primary Sense Practice Onboarding steps
- Primary Sense IT Provider Welcome Pack
Resources
- Primary Sense Quick Reference Guides
- Primary Sense training videos
- Primary Sense FAQs
- Data Security Poster
For registration and enquiries, please contact – PrimarySense@snhn.org.au
Resources
- Quality Improvement in Primary Care Guide
- Practice Incentive Payment Quality Improvement (PIP QI) – Service Australia
- Practice Incentives Program- Quality Improvement guidance
- Link to PDSA template
- Medical Director Data Cleansing Guide
- Best Practice Data Cleansing Guide
Enquiries – pcait@snhn.org.au
