COVID-19 information
This page contains advice for health professionals and community members on COVID-19 vaccination, and how to identify, manage and prevent the spread of COVID-19. Please note that the situation in Australia with regards to COVID-19 is changing rapidly and official local and national government sources will provide the most up-to-date information.
Adverse events
- Anaphylaxis: For GPs and practices undertaking vaccinations, before any vaccination session, check that you have the protocols, equipment and medicines to manage anaphylaxis. Please check you have an anaphylaxis response kit on hand. See anaphylaxis response kit for what is required.
- TGA Adverse Event Following Immunisation reporting form
Managing anaphylaxis after vaccination
The Australian Immunisation Handbook guidance on managing anaphylaxis after vaccination is available here.
The ASCIA resources on managing anaphylaxis are available here.
Myocarditis and pericarditis
This link provides detailed ATAGI advice.
Apply to administer Moderna Spikevax Moderna Bivalent, Nuvaxoid (Novavax), and Pfizer (Comirnaty) at your practice.
If you would like your practice to begin offering COVID vaccinations, please fill in the EOI form below:
EOI form to join the COVID vaccination program
General practices who are currently participating in the COVID-19 Vaccination Program can indicate their interest in receiving an ongoing allocation of the Moderna Spikevax Bivalent vaccine, and/or the Nuvaxovid (Novavax) vaccine, Pfizer (Comirnaty) vaccine.
To submit an Expression of Interest in your practice:
General information
- Department of Health: Information for COVID-19 vaccination providers
- ATAGI COVID-19 vaccine advice
- Health Pathways COVID-19 Vaccine Information
- NSW Health COVID-19 vaccines
Consent form
- Consent form for COVID-19 vaccination: click here
COVID-19 vaccine transfer
For full details on transfers, including how the vaccines should be transported, please read this information from the Department of Health.
After vaccination
Reporting vaccinations to the Australian Immunisation Register
It is now mandatory to report all National Immunisation Program (NIP) vaccinations to the Australian Immunisation Register (AIR).
From 1 July 2021, under the AIR Act, it is mandatory to report all NIP, COVID-19 and influenza vaccines administered to the AIR.
Immunisation providers can submit vaccination encounters to the AIR using:
- practice management software
- the AIR site via Health Professional Online Services (HPOS) using PRODA.
General immunisation training for providers
- Vaccine Storage and Cold Chain Management
- Immunisation Practice
- 347 Immunisation for Health Practitioners
- How to set up your access to AIR (Australian Immunisation Register)
Multicultural communications to patients and clients
- Department of Health: COVID-19 vaccine information in your language
VCF Connect will retire on 30 June 2023. As a part of the transition arrangements, the Department of Health and Aged Care are ceasing new registrations to VCF Connect as of Monday April 24.
What does this mean?
- Vaccine providers who have already registered in and claimed their services can continue to maintain vaccine services on the Service Finder through VCF Connect.
- Any vaccine provider that has not previously registered in VCF Connect will be able to get early access to Provider Connect Australia (PCA) to manage the vaccine services information.
- After VCF Connect is retired, all sites will be able to register in PCA and continue to self-manage their health services information.
The Department of Health and Aged Care and the Australian Digital Health Agency (ADHA) have worked together to offer COVID-19 Vaccine providers the opportunity to onboard to a new service called Provider Connect Australia.
COVID-19 information for health professionals
The Sydney North HealthPathways team have completed a rapid localisation of the pathway Coronavirus Disease (COVID-19) Information (including vaccination information). To request access to HealthPathways, or if you have any questions, please contact the HealthPathways Team: healthpathways@snhn.org.au
Updated information and advice for health professionals
- NSW Health guidance (includes FAQs, clinical advice, resources and more)
- Australian Government Department of Health website
- Home Care Guidelines for Adult Patients with mild COVID-19
Supporting people with disabilities during COVID-19
COVID-19 outbreak preparation: Advice for GPs with patients in Aged Care Facilities
Click here to view the tip sheet. This document is the first in a series to support GPs working in residential aged care facilities (RACFs) and is designed to support involvement in RACF COVID-19 ou-break preparedness activities. It incorporates the expertise of a range of stakeholders including our local Emergency Response Outbreak Advisory Group GPs, Dr James Hardy and Prof Sue Kurrle, Geriatricians in Northern Sydney LHD.
Process for Residents Developing COVID-19 Symptoms
During Regular Hours
Northern Sydney Local health District (NSLHD) mobile ‘Swab Team’ is available to attend Residential Aged Care Facilities (RACFs) to complete COVID-19 swabbing. The ‘Swab Team’ can be contacted on 0438 613 273 during these hours:
- Monday to Sunday (7 days)
- 9am – 5pm
After Hours
Outside of these hours, NSLHD does not provide a mobile COVID-19 testing service.
If a RACF resident develops COVID-19 like symptoms outside of these hours, please implement the following recommendations:
-
- Contact the resident’s GP for medical advice and/or follow your usual after hours GP protocols.
- Isolate the resident and implement contact and droplet precautions.
- Utilise appropriate PPE.
- If the resident remains well enough to remain in the RACF, contact the ‘Swab Team’ at 9am the following day.
- If the resident becomes acutely unwell, requiring urgent medical attention, call an ambulance on 000 and advise that the resident is potentially COVID-19 positive.
Guidelines for Aged Care Facilities on COVID-19 outbreaks – Department of Health
COVID-19 Vaccination for Aged Care Information
- COVID-19 vaccination – Aged care stakeholder kit: https://www.health.gov.au/resources/collections/covid-19-vaccination-aged-care-stakeholder-kit
- Reporting of clinical incidents: Vaccine Operations Centre (VOC): 1800 318 208 (7 days, 7 am-10 pm AEDT)
- Triaging and Directing Enquiries: https://www.health.gov.au/resources/publications/covid-19-vaccination-triaging-process-for-aged-care-facilities
- Guidance for monitoring side effects of COVID-19 vaccines: https://www.health.gov.au/resources/publications/covid-19-vaccination-monitoring-and-reporting-side-effects
Helping patients with Dementia navigate COVID-19
- National Dementia Helpline, 1800 100 500 – for all health professionals supporting people living with dementia, and family carers in need of support.
Guidance for RACFs on the public health management of acute respiratory infections (including COVID-19, influenza and RSV)
MBS telehealth arrangements
From 1 July 2022, ongoing MBS telehealth arrangements remain in place and provide for a wide range of telephone and video services by qualified health practitioners and support safe and equitable telehealth services which are informed by the MBS Review Taskforce Principles. Previous temporary arrangements ceased on 30 June 2022.
- Click here for an outline and factsheets concerning MBS telehealth and phone consultation item numbers.
We can help you set up telehealth technology in your practice
SNHN can help primary care practitioners and specialists get set up with a free, fit-for-purpose telehealth solution designed for health professionals. Email your query to digitalhealth@snhn.org.au
Process for prescribing during telehealth consults
The Department of Health has issued a ‘Guide for Prescribers’ fact sheet, containing arrangements for prescriptions to support telehealth services.
Video: how to use personal protective equipment (PPE)
View full version here (7 mins)
Other helpful links:
Do I need to get tested for COVID-19?
Anyone with COVID-19 symptoms should get tested.
People with coronavirus may experience any of the following:
- fever
- cough
- tiredness (fatigue)
- sore throat
- shortness of breath
- loss of taste or
- loss of smell.
If you have COVID-19 symptoms you can:
Stay protected in 2024: Your guide to COVID-19 vaccination
Ensure your ongoing protection against COVID-19 by understanding the latest vaccination guidelines for 2024.
As with all vaccinations, people are encouraged to discuss the vaccine options available to them with their health practitioner. You can also use the booster eligibility tool to determine whether you are eligible for a COVID-19 booster vaccination.
75 years and older
- Recommended every 6 months.
65-74 years
- Recommended at least every 12 months, but can receive every six months. Talk to your healthcare provider about the risks and benefits.
18-64 years
- With severe immunocompromise: Recommended at least every 12 months, but can receive every six months. Talk to your healthcare provider about the risks and benefits.
- Without severe immunocompromise: Can receive every 12 months.
5-17 years
- With severe immunocompromise: Can receive every 12 months.
- Without severe immunocompromise: Not recommended.
Under 5 years
- Not recommended.
See the Department of Health’s “COVID-19 vaccine advice for 2024” for further information.
Click here to access the Vaccine Clinic Finder.
If you don’t want to use the Vaccine Clinic Finder above to book, other ways to make a COVID-19 vaccination booking include:
- Book a vaccination at a local pharmacy.
- Call your GP to see if they offer COVID-19 vaccinations
- Why should I get vaccinated for COVID-19?
- COVID-19 vaccines – Is it true? – your questions and concerns answered.
Find information on COVID-19 vaccines for…
- pregnant and breastfeeding women: click here
- Aboriginal and Torres Strait Islander people: click here
- people with a disability: click here
- people with chronic health conditions: click here
- aged care residents and their families: click here
- frail older people, including those in residential aged care facilities (information about COVID-19 vaccines and vaccination decisions): click here
- Everyone in Australia aged 5 years and over is eligible: click here.
- Children aged 6 months to 5 years: click here
Before vaccination
- For information on what to do before you get vaccinated click here.
- COVID-19 Vaccination Consent Form
- Easy read consent form from the Department of Health
After vaccination
- COVID-19 Vaccine Side Effect Checker
- Find out what you need to do after you are vaccinated for COVID-19
The Therapeutic Goods Administration have created a COVID-19 vaccine information page for consumers and health professionals which answers common questions about how the TGA assesses and monitors a vaccine for safety, quality, and effectiveness.
You can get an immunisation history statement or digital certificate to show proof of your coronavirus (COVID-19) vaccinations. Click here to find out how.
If you have disabilities or elderly and unable to leave home, we provide an in-home service. Please email sneoc@snhn.org.au for further details on this.
The Northern Sydney Local Health District has made a vaccination sedation service available for young individuals requiring sedation to receive a COVID vaccination, located at the Royal North Shore Hospital Child and Adolescent short stay unit.
This service is available for any individual under 15 years and 11 months, however they can prioritise anyone above that age if necessary.
Referrals should be sent to NSLHD-vaccinationsedationintake@health.nsw.gov.au, and the anaesthetist and nursing team will review them.
If you’ve received a TGA-approved or TGA-recognised COVID-19 vaccine outside of Australia, and you received it on or after 1 October 2020, you can have it recorded on the Australian Immunisation Register (the AIR) when you return to Australia. It will then appear on all of the following:
- your COVID-19 digital certificate
- your International COVID-19 Vaccination Certificate
- your immunisation history statement.
Find more details here about having your COVID vaccines recorded on the AIR: https://www.servicesaustralia.gov.au/individuals/subjects/getting-help-during-coronavirus-covid-19/covid-19-vaccinations/how-get-help-proof/help-adding-overseas-vaccinations
COVID-19 information for community members
From 1 October 2023, positive COVID-19 rapid antigen test (RAT) results will no longer be registered with Service NSW. The RAT registration portal will close on this date.
- NSW Health still recommends you should stay at home and not visit high risk settings such as aged care facilities and hospitals if you have cold or flu symptoms. This is to help protect other people. Find out what to do if your RAT is positive or negative.
- If you are at higher risk of severe illness from COVID-19, speak to your doctor and make a plan about testing and antiviral medicines before you get sick. If you are unwell and can’t contact your doctor, call healthdirect on 1800 022 222 or use the online Service Finder.
- Free rapid antigen tests will no longer be available at Service NSW locations from 1 October 2023. Rapid antigen tests can still be purchased at pharmacies and supermarkets.
Older people or those with high risk of severe disease are also encouraged to speak to their doctor or vaccination provider about their COVID-19 booster vaccination.
Where can I find trusted sources of information?
Whilst media coverage of COVID-19 can help you feel informed, it can also trigger feelings of anxiety and agitation. To stay up to date with accurate, factual information you can access:
- AHPPC statement on COVID-19 winter update and ongoing health protection measures to support our community
- NSW Government COVID-19 webpage: gov.au/covid-19
- Service NSW App (available in the Apple App Store or Google Play)
- The Australian Government Department of Health Coronavirus Australia App (available in the Apple App Store or Google Play)
- The Australian Government’s WhatsApp channel on iOS or Android for official advice and information in real-time
- Australian Government Department of Health website: health.gov.au
Sometimes the information provided by the NSW Ministry of Health and Australian Government Department of Health may differ. This is because the NSW Government provides information specifically for NSW, which has the highest number of confirmed cases of COVID-19. The Australian Government provides information which is relevant for the whole of Australia – as a result, their messages may not be identical.
Multilingual Resources
NSW Health COVID-19 Information and resources in languages other than English
COVID-19 in-language resources from NSW Multicultural Health Communication Service
Translated resources for health workers and communities
Information from the Australian Government in your language Find information on health, education, business and financial support, visas and the border during the COVID-19 pandemic.
SBS Radio Coronavirus Information in Your Language
Australian Government Department of Health COVID-19 Fact Sheets
COVID-19 – What you need to know
COVID-19 – Information on social distancing
COVID-19 – Information about routine environmental cleaning and disinfection in the community
NSW Health and Australian Government Department of Health Information
NSW Health Novel coronavirus FAQs
Australian Government Department of Health Novel coronavirus (2019-nCoV) Information
Healthdirect
healthdirect website coronavirus (COVID-19) hub – first point of reference for reliable information about COVID-19
healthdirect Symptom Checker – an online tool that allows people to check their symptoms using a simple self-guided process.
Supporting people with disabilities during COVID-19
Person-centred emergency preparedness planning for COVID-19
- information on how to assist people with disability in planning for how they will manage the impacts of the pandemic
Coronavirus (COVID-19) hospital companion for people with disability
- information on how to assist a person with disability if they need to go to hospital
Coronavirus (COVID-19) – Information for Families
- information for families of a person with intellectual or developmental disability during the COVID-19 pandemic
Information for Disability Support Providers and Workers
- information and guidance for disability support providers and workers who provide health care to people with intellectual or developmental disability
Guide to personal protective equipment (PPE) for disability care providers
- information and guidance for disability care providers on the use of PPE
- information on who should be tested, where testing can be done, and how to explain the testing process to a person with disability
Most people who test positive for COVID-19 recover completely, but some people may develop long COVID. Long COVID is where symptoms of COVID-19 remain, or develop, long after the initial infection – usually after 4 weeks. It is not yet known how long symptoms of long COVID will last. In a large survey of people in the United Kingdom who had COVID-19, nearly 10% of people reported at least one symptom 12 weeks after their initial infection.
The Department has released a fact sheet on long COVID aimed at consumers. The links to the resources are below:
Preparing an anaphylaxis response kit (click here to download PDF)
Managing anaphylaxis after vaccination (click here to download PDF)
(Please note, the images above may not be the most up-to-date versions. Please click on the links above to ensure you access the most current PDF.)
NSW Health info sheet: anaphylaxis after vaccination
This NSW Health information sheet covers:
- signs and symptoms
- managing anaphylaxis
- risk factors for fatal anaphylaxis
ATAGI Site Requirements for COVID-19 Vaccination in Community Pharmacies
COVID-19 vaccination requirements in community pharmacies have been developed by the Australian Government in consultation with expert advice from the Australian Technical Advisory Group on Immunisation (ATAGI) and standards outlined in the Australian Immunisation Handbook. Identified/participating community pharmacies must confirm compliance with the minimum requirements prior to delivery of vaccine doses. Find requirements here: https://www.health.gov.au/resources/publications/covid-19-vaccination-site-requirements-for-covid-19-vaccination-in-community-pharmacies
NSW Pharmacist Vaccination Standards
The NSW Pharmacist Vaccination Standards have been further updated and published on the NSW Health website.
Online Training Resources
PRODA is an online authentication system providers use to securely access government online services such Australian Immunisation Register (AIR) and Health Professionals online Services (HPOS).
A PRODA account can be created by visiting the PRODA registration page here and selecting Register Now. You’ll need to complete the following steps:
- Create your account – you will need to provide personal details, create a username and password, and verify your email address.
- Verify your identity – you will need to verify your identity online using Government-issued identity documents e.g Australian Passport, Medicare card. A list of documents accepted can be viewed here.
- Link existing records – to gain access to services you’re eligible for as an individual such as HPOS, you’ll need to link your PRODA account to the service by clicking on the tile and enter any relevant details.
Recognised vaccination providers and administrators can use the AIR site through HPOS to record immunisation details for individuals, view and print immunisation history statements, request reports and update their contact details.
To download and print an immunisation history statement, please follow instructions here
OR
view our guide here.
NSW Health has developed a procedures guide around the cold chain management of the COVID-19 Vaccine AstraZeneca. This guide describes the process of receiving, storing, and administrating a COVID-19 vaccine. Click here to view.
Other useful resources
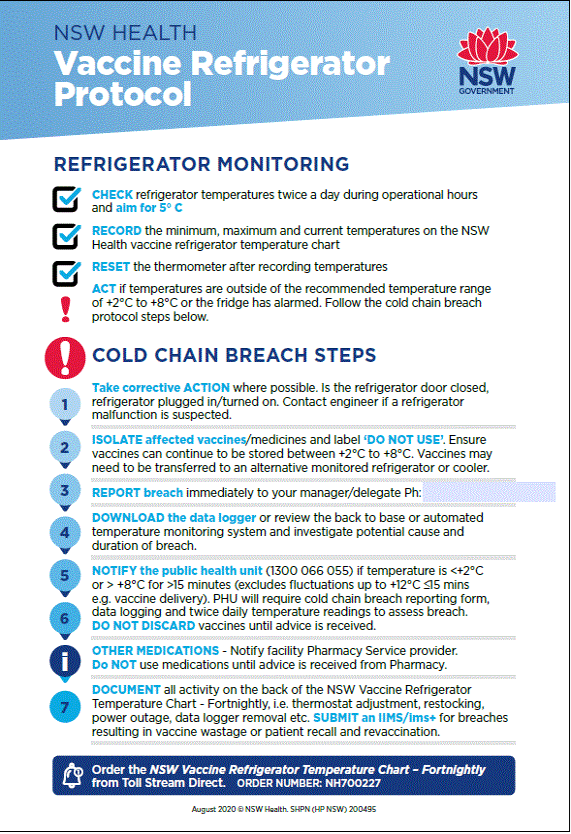
- Vaccine Refrigerator Protocol
- Pharmacy-specific cold chain management advice: https://www.qcpp.com/cold-chain-management
- NSW Cold Chain Breach Protocol
- Cold Chain Toolkit
- Strive for 5 guidelines
Click here to download the above infographic.
Practical infection prevention and control steps for patients, staff and managers in community pharmacies: please see info from NSW Health
All uncommon, serious or unexpected Adverse Event Following Immunisations (AEFIs) should be reported to your local public health unit.
To report a suspected AEFI, please complete the National Adverse Events Following Immunisation (AEFI) Reporting Form and contact your local Public Health Unit on 1300 066 055.
Further information: NSW Health – what is an AEFI?