Ageing Well
For more information please contact
ageingwell@snhn.org.au
For Health Professionals
Care finders is a national program delivered by all PHNs and funded by the Australia Government.
What do care finders provide?
Outreach and intensive one-to-one support to help vulnerable older people access My Aged Care, and connect to aged care and other relevant services. Care finders exists to support people who would not be able to access services without assistance. Care finders provide trauma-informed, inclusive care, and speak multiple languages.
How much does it cost?
This is a free, fully funded service for people who need extra, intensive support to access the care they need and other supports in the community.
Is this the right service for my patient?
To be eligible a patient must:
- have no carer or support person who can help them, or
- not have a carer or support person they feel comfortable or trust to support them, and
- be eligible for government-funded aged care.
In addition, they should have one or more of these reasons for needing intensive support:
- have difficulty communicating because of language or literacy problems.
- find it difficult to understand information and make decisions.
- be reluctant to engage with aged care or government.
- be in an unsafe situation if they do not receive services.
The eligibility criteria are flexible, and help is not means-tested. The program is mainly to help care recipients but, with permission, care finders can also work with carers or representatives.
Specific examples of who might be eligible to receive support from a care finder are:
- People who are uncomfortable with government due to past discrimination or trauma
- LGBTQIA+ community
- Forgotten Australians
- Care Leavers
- Refugees or migrants from conflict zones
- People with language barriers and no support
- People with cognitive impairments and no support
- People at risk of homelessness
- People at risk of elder abuse
- Veterans
- People struggling with dependence on alcohol and other drugs
- People living with mental illness
Find out more
The new DETECT Training module and materials are available at www.detect.snhn.net.
Sydney North Health Network & the Northern Sydney Local Health District has developed a new online training module for staff of residential aged care facilities, in collaboration with the Northern Sydney Local Health District Hospital Avoidance Teams (AART, APAC, BRACE & GRACE) on the Deteriorating Aged Care Resident.
- Palliative Care Needs Assessment (Sydney North Health Network, 2023)
- Flowcharts to assist GPs with specialist referrals (Palliative Care NSW)
- HELP app (an app to help yourself, or someone you care about, at end of life)
- Palliative Care Referral Form – HammondCare April 2018
- palliAGED GP Information Sheet & Links
- palliAGED Nurse Information Sheet & Links
- Nightingale Program: A specialist nurse-led support
and palliative care service promoting choice, wellbeing and forward planning available free of charge for people living with advanced dementia (in specific Australian locations)
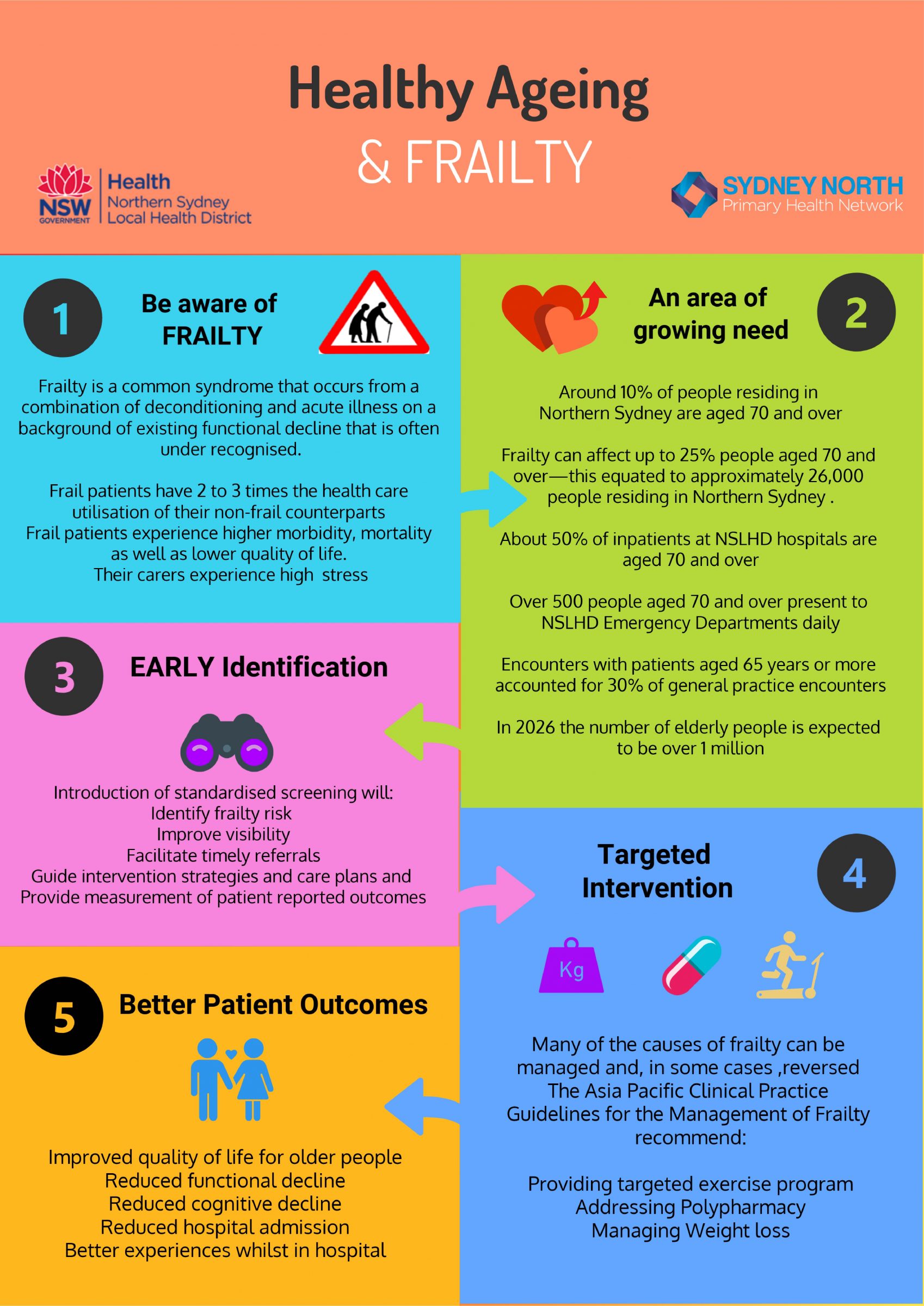
What is frailty?
Frailty is a common syndrome that occurs from a combination of de-conditioning and acute illness on a background of existing functional decline that is often under recognised. Many of the causes of frailty can be managed and, in some cases reversed to create better health outcomes and quality of life. It is therefore important to identify older people who are living with frailty.
How to identify frailty
Current health guidelines suggest that people over the age of 70 should be screened routinely.
In Northern Sydney we recommend the use of the The Frail Scale to identify a level of frailty.
A score of 1 to 2 indicates pre-frailty and a score of 3 or more indicates frailty.
Frailty is more common in females and the risk of frailty increases with age.
Identification and Management Quality Improvement Program
Then Sydney North Health Network (SNHN) invites practices to participate in the Frailty Identification and Management Quality Improvement Program (FIMQIP). The aim of the FIMQIP is to encourage and support general practices within SNHN’s catchment area to improve practice processes, resulting in better health outcomes for patients and provide sustainable quality improvement for General Practice. This will be achieved by identifying measurable and achievable key indicators within your practice setting.
View the “Frailty Management in Primary Care” Quality Improvement Toolkit.
How to manage frailty
Correctly managing frailty can significantly improve a person’s function and quality of life. It can also provide a better chance of recovery from acute illness as it reduces susceptibility to negative health outcomes.
Once you have assessed a person’s level of frailty (pre-frail or frail,) it is important to develop a management plan that addresses the corresponding sections of the frail scale.
This targeted approach can include:
- Referral to appropriate allied health professional such as a physiotherapist or dietitian
- Exercise classes
- Reviewing medications
- Managing weight loss
The decision support tool below provides more detail and some guidance for best course of action.
Frailty Management and Decision Support
Things to consider when implementing the Frail scale
Clinical Resources
The Best Practice and Medical Director templates
The Best Practice and Medical Director templates (.rtf files) can be imported to your software. These templates should not be opened and viewed before importing them. You will need to right click, copy and save or drag the .rtf file onto your desktop. Refer to the instructions below.
Frail Scale Templates for Medical Director
- Directions on how to upload templates
- Frail Scale for Medical Director (MD). To download, please Right Click and save link (clicking directly on this link will load the BP file into your web browser instead).
- 75+ assessment that includes Frail scale (MD). To download, please Right Click and save link (clicking directly on this link will load the BP file into your web browser instead).
Frail Scale Templates for Best Practice
- Directions on how to upload templates
- Frail Scale for Best Practice (BP). To download, please Right Click and save link (clicking directly on this link will load the BP file into your web browser instead).
- 75+ assessment that includes Frail scale (BP). To download, please Right Click and save link (clicking directly on this link will load the BP file into your web browser instead).
Other Resources
- Online Positive Aging Tool
- Suggested Management tool to accompany Frail Scale
- HealthPathways – Frailty Pathway
- Northern Sydney Frailty Initiative – Healthy Ageing and Frailty clinician brochure
- When Seniors Say No brochure
- Basic Steps (falls prevention program) resources order form
- Stepping On referral form
- Medication review for people living with frailty | Agency for Clinical Innovation (nsw.gov.au)
Evidence to Support Frail Scale:
- Asia Pacific Clinical Practice Guidelines for the Management of frailty
- Nutritional Interventions in Sarcopenia
- Effects of physical exercise interventions in frail older adults
- The Effectiveness of Exercise Interventions for the Management of Frailty: A Systematic Review
- Interventions for Treating Sarcopenia: A Systematic Review and Meta-Analysis of Randomized Controlled Studies
- Inappropriateness of Medication Prescriptions to Elderly Patients in the Primary Care Setting
- Beliefs and attitudes of older adults and carers about deprescribing of medications
Referrals
HealthPathways – For detailed clinical referral , assessment and management information related to the Northern Sydney region visit Sydney North HealthPathways site.
(Log in details are required and if you do not already have these please email healthpathways@snhn.org.au and they will be sent directly to you.)
Geriatrician – To refer to a Geriatrician for a comprehensive geriatric assessment please use the following:
- Search for a Geriatrician via postcode on Healthshare Open Search
- NSLHD Geriatrician referral
- Hornsby Ku-Ring-Gai Hospital – Ph: (02) 9477 9514 / Fax: (02) 9477 5684
- Royal North Shore Hospital Campus – Ph: (02) 9462 9333 / Fax: (02) 9906 4301
- Brookvale Community Centre – Ph: (02) 9998 6120 / Fax: (02) 9979 7876
- Mona Vale Community Centre – Ph (02) 9998 6120 / Fax: (02) 9979 7876
Geriatrician Outreach to Primary Care – aims to increase Geriatrician input into GP-led patient planning and care in the community while building relationships and facilitating two-way learning opportunities. It works with GPs to manage complex patients and prevent conditions that may be at potential risk of deterioration.
Search for Allied Health Professionals in Sydney North
Please use this search tool for Allied Health providers in Northern Sydney listed with an interest in frailty as registered in the Primary Health Network, this includes pharmacists that can assist with polypharmacy review.
Exercise
Active and Healthy Frailty prevention exercise program options in NSW
ViviFrail – for professionals responsible for the prescription of a program of physical exercise
Progressive resistance training for frailty
For patients requiring individual exercise prescription, a physiotherapist or exercise physiologist:
Australian Physiotherapy Association: Find a physiotherapist
Exercise & Sports Science Australia: Find an exercise physiologist
NSLHD outpatient Physiotherapy referral information
Dietary advice
NSLHD outpatient Dietitian referrals (accepts GP referral)
Home safety assessment and occupation therapy
- NSLHD outpatients
- Hornsby Ku-ring-gai Hospital Outpatients – Ph: (02) 9477 9493
- Northern Beaches Health Service – Ph: (02) 9998 6100
- Royal North Shore Hospital – Ph: (02) 9462 9666
- Ryde Hospital – Ph: (02) 9858 7888
Sydney Home Nursing Safe and Steady Program
Regal Home Health Ph: (02) 9264 4555 – Care coordination links to assist in conducting 75+ health assessments with patients
Falls can be prevented – help your older patients prevent falls and stay independent
Falls are common in older people but they can be prevented.
Do your older patients relate to either of the following risk factors?
- Having had a fall or worried about falling
- Unsteadiness when walking
- Conditions that impact mobility such as diabetes, stroke, arthritis
- Taking psychotropic medications
- Polypharmacy
- Poor vision
- Dizziness
- Urge incontinence
- Clutter in the home
Developing routine for fall prevention in general practice.
For more videos on the role of health professionals in preventing falls in older people please click here.
GP Resources
Prof Lindy Clemson and a team of multidisciplinary researchers including GPs have developed a clinical decision tool and resources based on the latest research evidence and practice guidelines.1-4 We anticipate that these will help GPs and practice nurses identify people at risk of falling and provide tailored management options. GPs are also offered a directory of trained fall prevention service providers in their local area to facilitate patient referral.
The clinical decision tool, resources, and referral directory are now available online through the iSOLVE tool button below. Please contact Alex Jaksetic by email ajaksetic@snhn.org.au if you would like educational visiting to be organised.
Find a Falls Prevention Provider
Download resources
- Decision tool for fall prevention in general practice patients 65+
- Patient Stay Independent checklist (fillable PDF)
- GP fall risk assessment (fillable PDF) and tailoring interventions to fall risk factors
- Provider resource (fact sheets, MBS summary, case studies, talking with patients)
- Poster for waiting room
- Letter writer template for MedicalDirector and BestPractice – please import and save into your clinical software before opening.
- Other resources
Education
- GP online active learning module and clinical audit activities
- Top tips from local health professionals: Topic: Falls Prevention – Speakers: Megan Swann, Mary Potter, Dr Nick Bernard
- Fall prevention webinars: falls.armchairmedical.tv
Software partnership
- Decision tool, information and resources within SNPHN HealthPathways
- HotDoc reminder to prompt patients to discuss with their GPs or practice nurses about preventing falls
Allied Health Resources

SNHN offered various workshops to health service providers to facilitate referral pathways and implementation of evidence-based fall prevention interventions. SNHN will continue to promote future fall prevention workshops through the Education Events page. You may wish to view some of the recorded workshops here: www.falls.armchairmedical.tv.
If you are a community-based service provider and have undertaken fall prevention training with SNHN or another organisation, you may wish to be listed as a provider for patient referral from GP practices for interventions relevant to your practice. To express interest please contact Alex Jaksetic by email ajaksetic@snhn.org.au.
Advance Care Planning is a series of steps to help patients plan for their future healthcare. Studies conducted in a range of healthcare settings suggest that advance care planning can improve individual and family satisfaction with care, reduce the number of people transferred from nursing homes to hospitals, as well as reduce stress, anxiety, and depression in surviving relatives.
- Advance Care Planning brochure for GPs – helping your patients to make their wishes known
- RACGP
- Aboriginal and Torres Strait Islander discussion starter
Templates
Dementia is now the leading cause of disease burden for older Australians*. With an ageing and growing population, it is predicted that the number of Australians with dementia will more than double by 2058 to 849,300. However, it doesn’t just affect the person living with dementia – it also affects carers, friends and family.
Diagnosing dementia can be difficult due to the insiduous onset of the disease. Recognising the early signs can be challenging in a primary care setting, and patient denial of cognitive changes can further complicate the picture.
Yet, striving for an early diagnosis is important, and GPs can do this effectively with the right probing, investigations and cognitive testing.
Sydney North Health Network is offering the Dementia Quality Improvement Program to all General Practices in the region. The program provides support to participating practices to analyse current dementia care management and develop individualised plans to support implementation of evidence-based best practice care.
For more information or to express an interest to participate in the Dementia Quality Improvement Program, please complete this Expression of Interest form.
Identifying and Managing Dementia
- Health Pathways Cognitive Impairment and Dementia
- Dementia Outcomes Measurement Suite – compendium of validated tools for the assessment of various aspects of dementia
- Clinical Practice Guidelines- Cognitive Decline Partnership Centre
- A Care Guide for General Practice
- 14 Essentials for Good Dementia Care in General Practice
- Early Dementia – Optimal Management in General Practice
- AIHW: Dispensing patterns for anti-dementia medications 2016-17
- Dementia, decision aids and general practice
- Advance Care Planning and Dementia
- Dementia in Residential Aged Care: A guide for care workers
- Dementia and Driving
- GP Advice Service – GPs can access clinical advice from geriatric team specialising in dementia management
- Nightingale Program – offered free of charge, this is a specialist nurse-led support and palliative care service promoting choice, wellbeing and forward planning
News and education
- University of Tasmania Wicking Dementia Research and Education Centre
- Dementia Training Australia
- Dementia In Practice Podcast Series for Health Professionals
- The Dementia Podcast
- Future Planning and Advance Care Planning Report: Why it needs to be different for people with dementia
- Future Planning and Advance Care Planning Companion Document
Health Professional and Patient Support Services
Dementia Australia Services
- Post diagnostic support program: 6 sessions over 12 months to enhance understanding, plan support and plan and prepare for changes
- Individual and family based Counselling support – face to face, on the phone or via videoconferencing
- Living with Dementia group program – Interactive program provides an overview of dementia and how to proceed after a diagnosis. It covers coping with change, relationships, and communication, planning for the future, and staying healthy.
- Library of resources – including factsheets, books, ebooks and video content
Other services
- Dementia Behaviour Management Advisory Service (DBMAS) 24 hour over the phone advice when there are complex behaviours that are stressful for a Carer to manage. They can help the Carer work out strategies and access appropriate medical care. Phone 1800 699 799
- Proveda Northern Sydney Dementia Advisory Service provides advice and assistance to people with dementia and their families and can link them with other people with dementia and their carers. Phone 1300 002 262
- National Dementia Helpline – Free 24 hour telephone service providing information and advice to people with dementia and their friends and family and health and aged care workers. They can also connect to Dementia Australia and community support services and program and discuss government support, including My Aged Care, NDIS, Carer Gateway and DBMAS.
Phone 1800 100500.Webchat: dementia.org.au/helpline/webchat. Operating hours Mon – Fri 8am-8pm.
Dementia Apps
- Forward with Dementia – practical information and tools for healthcare professionals and patients
- My Dementia Companion – practical dementia tool to guide professionals and carers through the dementia journey
- Face Dementia patient resource to learn about the signs, recognise them in yourself or others, and start a conversation about visiting a GP to get help.
Brain training apps
- BrainTrack app – BrainTrack is a free app that helps people monitor and understand changes in cognition over time, which can be used to start a conversation with their GP.
- Brain HQ
- Cognifit
- Happyneuron
- Neuronation
For Community Members
Northern Beaches Dementia-Friendly Community Project
The Advisory group is open to people living with dementia and their carers and has been set up to create a dementia-friendly community in the Northern Beaches.
Northern Beaches Dementia Alliance
NBDA consists of aged care, dementia, and healthcare professionals as well as community members, people living with dementia, and their carers. NBDA aims to increase awareness and understanding of dementia on the Northern Beaches, and to encourage dementia-friendly communities.
Northern Sydney Dementia Collaborative
The Northern Sydney Dementia Collaborative was established in 2014, with assistance from the NSW Agency for Clinical Innovation’s “Building Partnerships” program, which aimed to form alliances that work together to integrate care for older people with complex health needs. Nowhere is this more needed than in people with dementia. There are a range of services available in Northern Sydney for people with dementia and their carers. However, information about these services and how to access them is not well understood by the people who need them the most or by health professionals. It is estimated that over 12,000 people in Northern Sydney are living with dementia and this figure will continue to grow as the population ages.
Better Journeys for People with Dementia in Northern Sydney
Focus Area – Supporting providers to deliver care, and engaging older people and their carers through improving transparency and accessibility of available services.
In Australia, three in ten people over the age of 85 and almost one in ten people over 65 have dementia. In Northern Sydney, there is projected growth of 23% in the population of people aged 75 years and older between 2011 and 2021, indicating a substantial increase in the number of people with dementia in the region over the next 6 years. In addition, there are approximately 24,700 people in Australia with Younger Onset Dementia (a diagnosis of dementia under the age of 65; including people as young as 30).
On average symptoms of dementia are noticed by families three years before a firm diagnosis is made. The journeys of many people with dementia and their carers include points of contact with the health system with an absence of helpful advice or information about services, and a series of points of stress, pain or crisis. People with dementia are relatively high users of acute hospitals. In Australia the mean LOS for all hospital separations is 8.6 days, compared with a mean of 19.6 days for any diagnosis of dementia and 30.1 days for separations with a principle diagnosis of dementia (Draper 20071).
This work will also include health promotion including brain health, building capacity in General Practice and working together to promote advanced care planning for the benefit of people with dementia and their carers in Northern Sydney.
It is expected that with access to this information people with dementia will have better plans in place to manage their care, more timely access to support, and there will be reduced unplanned admissions to hospital for people with dementia.
A partnership between Northern Sydney Local Health District, Sydney North Health Network, Community Care Northern Beaches, and Dementia Australia NSW will be developing a dementia pathway which will provide guidance around appropriate services, with information regarding how to access these in the region.
The Collaborative includes representatives from SNHN, Northern Sydney Local Health District, Dementia Australia Community Care Northern Beaches, Northern Sydney Regional Dementia Advisor, local GPs and a carer with lived experience caring for a family member with dementia. This group aims to develop strategies to improve the healthcare journey for people with dementia and their carers. This includes:
- Creation and extensive distribution of the “Memory Problems” brochure which provides both consumers and health professionals with essential local service information.
- Development of a cognitive impairment pathway – one of Northern Sydney’s first HealthPathways.
- Co-design of a discharge follow-up service to support transition from hospital to home for people at high risk of readmission.
- Education events for health professionals, carers and consumers.
- Working in partnership to develop dementia friendly communities.
- Supporting the efforts of local councils to develop dementia friendly communities, as well as supporting health care services to be more dementia friendly.
It is expected that with access to this information, people with dementia will have better plans in place to manage their care, more timely access to support, and there will be reduced unplanned admissions to hospital for people with dementia.
1 Draper et al (2007) Hospital Dementia Services Project: Dementia Services Provided in Public Hospitals, NSW, Australia, downloaded via AIHW website, contact Brian Draper; b.draper@unsw.edu.au.
PACE Early Intervention Program
Are you or a loved one worried or feeling overwhelmed about a recent diagnosis? Not sure of the next steps?
PACE, commissioned by the Sydney North Health Network, aims to help you or a loved one who has recently been diagnosed with a chronic condition or are at risk of developing one.
The PACE program provides 1:1 support and information about your diagnosis and symptoms. It connects you to the right services and groups that enable healthy ageing and management of chronic conditions.
A dedicated ‘PACE Partner’ will provide ongoing support to help guide and connect you with various providers or community groups (e.g. home care, physio, social support).
Available Monday – Friday 9.00am – 5.00pm. Will accept medical, nursing, allied health and self-referrals.
To register or make a referral, please contact us using the details below.
Ph: 0484 021 880 / 02 9988 4966
W: https://www.knc.org.au/contact-8
Community Transport Early Intervention Pilot Program
The Community Transport Early Intervention program funded by SNHN helps older Australians get to their health appointments and social wellbeing activities, enabling them to stay healthy and independent for longer.
To be eligible for this free program, a participant must:
- live in any of the Local Government Areas (LGAs) in the Northern Sydney region
- be aged over 65 years, or 40 years or over for Aboriginal and Torres Strait Islander Peoples
- not currently be accessing community transport through My Aged Care.
Call: 1800 035 262
Website: https://www.cto.org.au/cto-projects/earlyintervention/
care finders
Care finders is a national program delivered by all PHNs and funded by the Australia Government.
What do care finders provide?
One-to-one support to help vulnerable older people access My Aged Care, and connect to aged care and other relevant services. Care finders exists to support people who would not be able to access services without assistance. Care finders provide trauma-informed, inclusive care, and speak multiple languages.
How much does it cost?
This is a free, fully funded service for people who need extra, intensive support to access the care they need and other supports in the community.
Specific examples of who might be eligible to receive support from a care finder are:
- People who are uncomfortable with government due to past discrimination or trauma
- LGBTQIA+ community
- Forgotten Australians
- Care leavers
- Refugees or migrants from conflict zones
- People with language barriers and no support
- People with cognitive impairments and no support
- People at risk of homelessness
- People at risk of elder abuse
- Veterans
- People struggling with dependence on alcohol and other drugs
- People living with mental illness
Find out more
- Northern Sydney Local Health District – Carer Support Service
Call on: 02 9462 9488
- Carer Gateway
Call on: 1800 422 737
Carer Gateway is a national online and phone service that provides practical information and resources to support carers. The interactive service finder helps carers connect to local support services.
Complete your own online positive ageing screening.
Healthy eating to stay strong and independent
Stepping On brochure (falls prevention program)
Meals on wheels contact numbers:
- Crows Nest – Ph: (02) 9437 7517
- Hornsby Ku-Ring Gai – Ph: (02) 9144 2044
- Hunters Hill Ryde – Ph: (02) 9817 0101
- Lane Cove – Ph: (02) 9427 6425
- Mosman – Ph: (02) 9978 4130
- Willoughby – Ph: (02) 9777 7830
- Manly – Ph: (02) 9976 1469
- Northern Beaches – Ph: (02) 9970 8399
NSLHD Health Contact Centre – Ph: 1300 732 503 (Mon-Fri: 7.30 am to 6.30pm)
NSLHD Carer support information website
LiveUp is a free national healthy ageing platform designed to help you reimagine, reset, and reconnect with living your life to its fullest. You’ll find personalised suggestions, including tailored activities, assistive products, social connections, and more, all in your local area or online.
- NSW exercise venues (Active and Healthy website)
- Staying Active and On Your Feet booklet
- Example of balance exercises
- Example of foot and ankle exercises
- Fall prevention patient flyers
- Staying Power: Tips and tools for keeping you on your feet – Sydney University Press
Many people who live with Dementia continue to make their own choices and live rich and active lives but Dementia Australia’s research shows that there is a prevailing attitude that people living with dementia are old, frail and living in care.
Dementia affects almost half a million Australians and that number is estimated to double over the next 25 years. As something that will impact the lives of many Australians and their friends and family in the future we must work together to improve the care and wellbeing of those living with this disease and support people living with dementia to live well for as long as possible.
How do I reduce my risk?
Keeping your brain healthy is essential for living a fulfilling, healthy life. In fact, scientific research suggests that a brain-healthy lifestyle can reduce your risk of developing dementia later in life.
Whether you are young or old, there are simple changes you can make to improve and protect your brain health:
Dementia Australia Healthy Brain Healthy Life Booklet
SNHN Dementia Risk Reduction Factsheet
Brain training apps
BrainTrack app – BrainTrack is a free app that helps people monitor and understand changes in cognition over time, which can be used to start a conversation with their GP.
I am having memory problems
Early diagnosis is important. It can help you and your carer to understand what is happening and why, and to get the support and services you need.
If you are concerned about yourself or someone you know experiencing symptoms of memory loss or confusion it is important to have a conversation with your GP. They may organise some tests and you may be referred to specialists such as a geriatrician, psychogeriatrician or neurologist for further assessment and diagnosis.
- Memory Problems: Information for people with Dementia and their carers
- CDPC: Dementia Consumer Guide
Dementia Apps
- Forward with Dementia – practical information and tools for healthcare professionals and patients
- My Dementia Companion – practical dementia tool to guide professionals and carers through the dementia journey
Face Dementia patient resource to learn about the signs, recognise them in yourself or others, and start a conversation about visiting a GP to get help.
Dementia support and carer support
 Memory Problems: Information for people with Dementia and their carers
Memory Problems: Information for people with Dementia and their carers- CDPC: Dementia Consumer Guide
Dementia Australia Services
- Post diagnostic support program: 6 sessions over 12 months to enhance understanding, plan support and plan and prepare for changes
- Individual and family based Counselling support – face to face, on the phone or via videoconferencing
- Living with Dementia group program – Interactive program provides an overview of dementia and how to proceed after a diagnosis. It covers coping with change, relationships, and communication, planning for the future, and staying healthy.
- Library of resources – including factsheets, books, ebooks and video content
- Nightingale Program – offered free of charge, this is a specialist nurse-led support and palliative care service promoting choice, wellbeing and forward planning for people living with dementia
Local Support Services
- Dementia Behaviour Management Advisory Service (DBMAS) 24 hour over the phone advice when there are complex behaviours that are stressful for a Carer to manage. They can help the Carer work out strategies and access appropriate medical care. Phone 1800 699 799
- Proveda Northern Sydney Dementia Advisory Service provides advice and assistance to people with dementia and their families and can link them with other people with dementia and their carers. Phone 1300 002 262
- National Dementia Helpline – Free 24 hour telephone service providing information and advice to people with dementia and their friends and family and health and aged care workers. They can also connect to Dementia Australia and community support services and program and discuss government support, including My Aged Care, NDIS, Carer Gateway and DBMAS.
Phone 1800 100500.Webchat: dementia.org.au/helpline/webchat. Operating hours Mon – Fri 8am-8pm.
Supporting Carers
- Northern Sydney Local Health District – Carer Support Service
Call on: 02 9462 9488 - Carer Gateway
Call on: 1800 422 737
Carer Gateway is a national online and phone service that provides practical information and resources to support carers. The interactive service finder helps carers connect to local support services.
Local Dementia-friendly Councils and Communities
Dementia-friendly cafes and support groups promote social inclusivity for those living with dementia, as well as their friends, relatives and carers. Those who live with dementia can often feel isolated and lonely so these spaces have been created to encourage people with shared experiences to meet.
Get in touch with your council or local Dementia Alliance to access a number of local resources for older people and those living with dementia and their carers.
Planning for the future
Advanced Care Planning
Advance care planning involves talking about your values and the type of health care you would want to receive if you became seriously ill or injured and were unable to say what you want.
https://sydneynorthhealthnetwork.org.au/programs/aged-care/#1691456949057-62a3debb-296d
Enduring Guardianships and Power of Attorney resources
A guardian (who could be a family member or friend), is a substitute decision maker who may make lifestyle decisions, such as where a person should live, as well as give their consent to medical, dental and health care services.
https://ncat.nsw.gov.au/how-ncat-works/ncat-divisions-and-appeal-panel/guardianship-division.html
Financial Advice
When planning your finances for aged care, there are many aspects to consider—for example, pensions, superannuation, and retirement planning. So, it is beneficial to seek independent financial advice before deciding how to pay for your aged care.
The My Aged Care website has a great deal of information to support your needs.
https://www.myagedcare.gov.au/financial-support-and-advice
Palliative Care
Palliative Care is care and support provided to people who have a progressive, life-limiting illness. A life-limiting illness is an illness that cannot be cured. There are many life-limiting illnesses such as cancer, motor neurone disease, end-stage heart failure, end-stage lung or kidney disease and dementia. The focus is on improving the quality of life of patients, their families, and carers by addressing their many needs; physical (including treatment assessment and management of pain and other symptoms), emotional, social, cultural, and spiritual need.
Palliative Care NSW – https://palliativecarensw.org.au/families-and-carers/resources/
Sydney North Health Network Palliative Care link and resources https://sydneynorthhealthnetwork.org.au/programs/aged-care/#1691457232142-83ec5247-6a7a
For more information on palliative care services available in your local area, ask your GP, or contact the National Palliative Care Service Directory.