Person-Centred Care Program
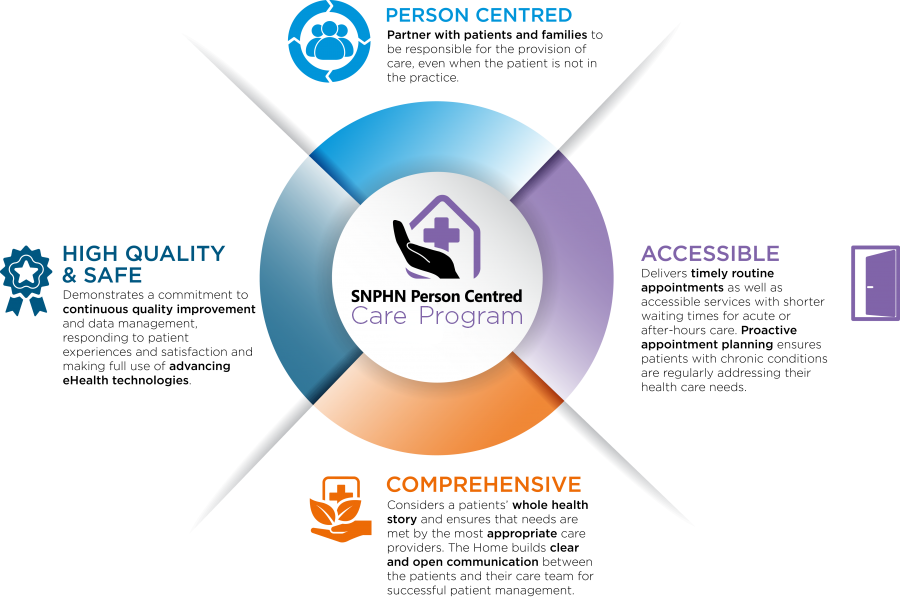
A Person-Centred Care approach combines the traditional core values of family medicine – providing comprehensive, coordinated, integrated, quality care – that is easily accessible and based on an ongoing relationship between a person and their health care team.
The Person-Centred Care Program aims to assist practices with small step-by-step changes they choose to make. Practices are invited to participate in a range of person-centred care initiatives, which are offered throughout the year.
Practice benefits:
- Access to education and resources for practice staff new to Person Centred Care Programs
- Leadership training and coaching
- Focused quality improvement practice tools
- Regular in-practice support
- Access to a network of local general practices who have previously or are currently participating in program
- Increased efficiencies in preventive healthcare and chronic disease management
- Increased efficiencies in MBS item number billing
- Improved work life and professional satisfaction for clinicians
- Enhanced quality care and experience for patients
Key Principles
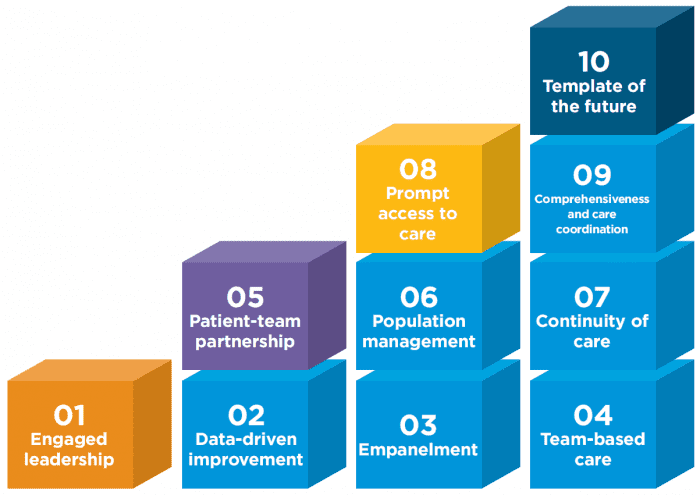
Building Blocks
1. Engaged Leadership
How well do you know your leadership style and the effect it has on your health care team? Everyone is a leader, however in the medical home General Practitioners are central to the success of driving change and achieving outcomes.
2. Data-Driven Improvement
Using a data extraction tool alongside clinical software to understand the practice patient population is invaluable when managing the requirements of the person centred medical home. Make data part of the work life.
3. Empanelment (Patient Registration)
This involves linking each patient with a primary care provider and care team. To improve continuity and establish a strong patient-team partnership it is important that patients and the care team know each other and plan the care together.
4. Team-Based Care (Building the Team)
Creating more effective practice teams is the key to becoming a patient-centred medical home, improving patients’ health, and increasing productivity. A team-based approach can lead to markedly improved care, efficiency, and job satisfaction.
5. Patient-Team Partnership
An effective partnership recognises the expertise that patients bring to the medical encounter as well as the evidence base and medical judgment of the clinician and team. Patients are not told what to do but are engaged in shared decision making that respects their personal goals.
6. Population Management
High-performing practices stratify the needs of their patient panels and design team roles to match those needs. Three population-based functions provide major opportunities for sharing the care: panel management, health coaching, and complex care management.
7. Continuity of Care
Is associated with improved preventive and chronic care, greater patient and clinician experience, and lower cost. To achieve continuity requires empanelment linking each patient to a clinician and team.
8. Prompt Access to Care
Access is linked to patient satisfaction and is a prominent objective for many practices. Though the science of access is well-developed, practices frequently fail in their efforts to reduce patient waiting time.
9. Comprehensiveness and Care Coordination
Refers to the capacity of a practice to provide most of what patients need. Another pillar – care coordination – is the responsibility of primary care to arrange for services that primary care is unable to provide.
10. Template of the Future
Few practices have achieved this ultimate goal: a daily schedule that does not rely on the 15-minute in-person clinician visit but offers patients a variety of e-visits, telephone encounters, group appointments, and visits with other team members.
Education and Resources
Covering a range of topics, this 5-part webinar series aims to equip practice staff with enhanced knowledge for growing a thriving, high-performing general practice.
Webinar 1: Reaching Business and Financial Potential
Presented by: David Osman, Practice Manager; Healthcare Trainer; and Board Director, AAPM
Webinar air date: Wednesday 18 August 2021
View webinar recording
Webinar 2: Communication Essentials for Frontline Staff
Presented by: Gary Smith, Practice Manager; Practice Manager; Chair, Quality Innovation Performance Limited (QIP)
Webinar air date: Tuesday 21 September 2021
View webinar recording
Webinar 3: Striving for Continuous Quality Improvement
Presented by: Gary Smith, Practice Manager; Practice Manager; Chair, Quality Innovation Performance Limited (QIP)
Webinar air date: Wednesday 13 October 2021
View webinar recording
Webinar 4: Optimising Teamwork and Collaboration
Presented by: Tracey Johnson, Chief Executive Officer, Inala Primary Care; Deputy Chair, Primary Care Advisory Group, AIHW
Webinar air date: Tuesday 16 November 2021
View webinar recording
Webinar 5: Person-Centred Health System and Integrated Care
Presented by: Tracey Johnson, Chief Executive Officer, Inala Primary Care; Deputy Chair, Primary Care Advisory Group, AIHW
Webinar air date: Thursday 2 December 2021
View webinar recording
Enquiries
Primary Care Advancement Team
T: (02) 9432 8250, E: pcait@snhn.org.au