GP News – July ’16
Contents
- GPs required for new study to screen for Atrial Fibrillation using a smartphone ECG
- After-hours helpline for palliative patients and carers
- One million people see a GP for mental illness every year
- Linking hepatitis C patients with GPs and pharmacies
- Improvement to the My Aged Care web referral form
- How My Aged Care can help your patients
- NSW Authorised Care Plans for GPs
- Memory Problems? – A new resource for people with dementia and their carers!
- New Lung Foundation Australia Lung Cancer Resources for Patients and Health Professionals
- Treating and managing dysphagia and how to refer to a Speech Pathologist
- Revision of the healthy blood pressure guidelines
- Making innovative use of cohort data to inform health service delivery
GPs required for new study to screen for Atrial Fibrillation using a smartphone ECG
Sydney North Health Network is working with the University of Sydney to recruit general practices to take part in a study to screen for Atrial Fibrillation (AF) using a smartphone ECG.
This information sheet was provided by Professor Ben Freedman OAM, Professor of Cardiology, University of Sydney, which can be accessed CLICK HERE.
Participating clinics receive all devices and software, $1000 to cover setup costs and $10 per patient for the first 500 patients screened. If you are interested in participating or would like more information, please contact The Primary Care Advancement and Integration Team e: pcait@snhn.org.au or ph 9432 – 8250.
CLICK HERE for the article “iPhone ECG screening by practice nurses and receptionists for atrial fibrillation in general practice: the GP-SEARCH qualitative pilot study”.

After-hours helpline for palliative patients and carers
An after-hours helpline to support people receiving palliative care, their carers and health professionals was recently launched by Health Minister Jillian Skinner.
The Palliative Care After-Hours Helpline is part of the NSW Government Plan to Increase Access to Palliative Care.
The helpline is staffed by registered nurses with training in palliative care. If the issue is more complex, the call is transferred to a specialist palliative care nurse. Support provided can include information about symptoms, pain and medication management, advice on how to manage equipment and emotional support to manage fears.
It is available on weeknights (5pm – 9am), weekends (5pm Friday to – 9am Monday) and on public holidays.
The Palliative Care After-Hours Helpline is a free call number – 1800 548 225.
CLICK HERE for more information about the helpline.

One million people see a GP for mental illness every year
More than one million people accessed MBS mental health services via a GP in 2011, according to a new report from the Australian Bureau of Statistics.
Only 316,000 people accessed similar services from other health professionals, although these people averaged about four extra consultations compared with those who saw a GP.
About 2.35 million people, or 11% of the population, accessed PBS medications for mental health conditions in the same year.
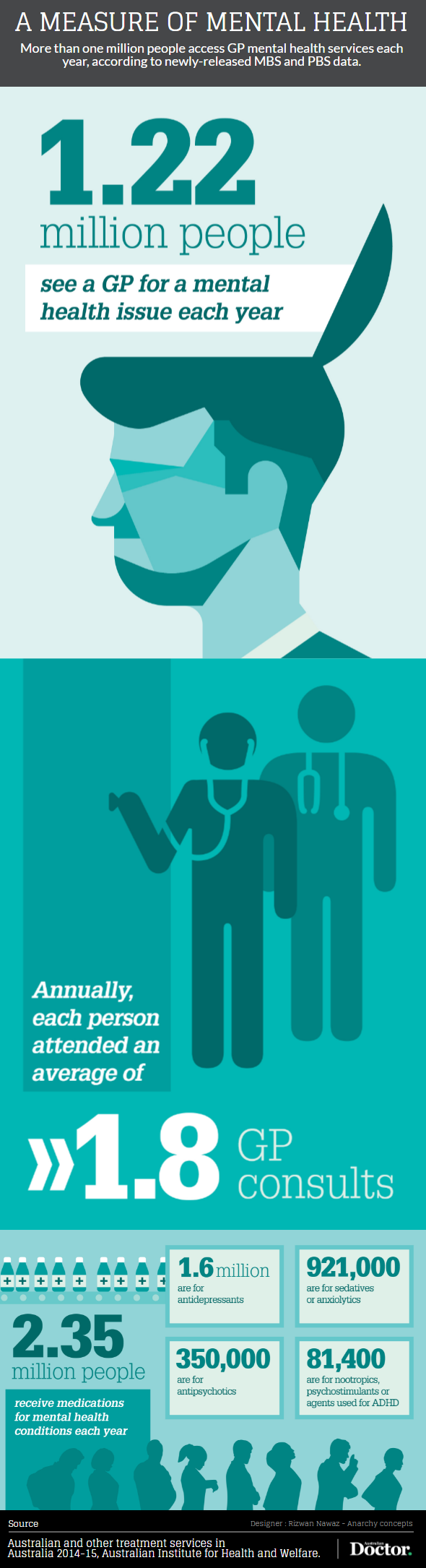
Source: Australian Doctor, Antony Schofield – 11th July 2016

Linking hepatitis C patients with GPs and pharmacies
Revolutionary treatments for hepatitis C are now available on the PBS. They can be prescribed by General Practitioners (in consultation with a gastroenterologist, hepatologist, or infectious disease physician experienced in the treatment of chronic hepatitis C infection).
The drugs are championed by Australian Minister for Health, The Hon Sussan Ley, and redefine hepatitis C as a relatively easy-to-treat health condition.
Over the past three months, Hepatitis NSW has been building an online web directory of GPs and pharmacies who work with the new drugs. Their aim is to link patients with their local service providers.
According to Hepatitis NSW “In the Northern Sydney PHN region we currently have only 9 GPs or chemists but we’d like to have many more.”
To be added to the directory, or if you’d like more information about the DAA drugs, please email pharvey@hep.org.au.
To view the directory CLICK HERE.
For more information on this initiative, CLICK HERE.

Improvement to the My Aged Care web referral form
A new web form that will assist healthcare professionals to refer patients to the My Aged Care system is now available for use, part of release five of the online assessment and referral system for Commonwealth-funded aged care services.
There have been significant changes which are intended to:
- Improve patient and referrer experience by reducing the time for inbound referral handling in the contact centre;
- Streamline the screening and assessment process by ensuring that accurate and more complete information is provided to assessors and service providers, reflective of information provided by the health professional when making the original referral;
- Enable the referrer to more easily follow-up on their referrals to My Aged Care by provision of a confirmation ID; and
- Achieve consistency in referral pathways.
The web referral form allows more information to be captured about a patient and enables health professionals to create a referral that will be processed automatically.
CLICK HERE for the referral form or call the contact centre on 1800 200 422 (open 8am to 8pm locally Monday to Friday and 10am to 2pm locally on Saturday).
Exceptional situations when a client may be accepted for service without an assessment
There are exceptional circumstances where a patient has an immediate need for personal care, nursing, transport or meal services and their safety could be at risk if the services do not start immediately. In these circumstances a health professional may refer to;
- A CHSP provider direct to start providing services before referring the client to My Aged Care; or
- My Aged Care contact centre who may directly refer the client for interim services while at the same time referring the client to the RAS.
To find a service with availability in your area use the My Aged Care Service Finder.
CLICK HERE for GP Referrals to My Aged Care Fact Sheet June 2016.

How My Aged Care can help your patients
On 1 July 2015, the Commonwealth changed the way older people access aged care services by introducing My Aged Care.
My Aged Care (MAC) is the first point of contact for individuals seeking information about aged care and access to aged care services. Hence it is likely to be relevant to many of your patients, particularly in the following situations:
- a family member is concerned about an older person and needs to understand the care options available
- a patient is presenting with a declining ability to manage their activities of daily-living and need to either plan for the future or access services now
- you have questions around the sustainability of a patient’s current care arrangements
It is important that clients are referred to My Aged Care to ensure their aged care needs can be assessed holistically and the right services put in place to support their needs, goals and service preferences.
For individuals who are already receiving aged care services, there is no need for them to register with My Aged Care. However, if their needs and/or circumstances change significantly, then they need to be registered.
How Do I Make a Referral to My Aged Care?
- Use the online ‘Make a Referral‘ form
- Call MAC on 1800 200 422 (8am-8pm weekdays; 10am-2pm Saturdays). The patient does not have to be present for a phone referral, however you will need your patient’s consent before you provide information on their behalf.
- Fax MAC on 1800 728 174
If you’d like to be kept up-to-date with what is happening in the Aged Care Sector, please subscribe to Northside’s Monthly eBulletin at http://www.nsforum.org.au/sector-support/ebulletin

NSW Authorised Care Plans for GPs
Did you know that 50% of patients attended by NSW Ambulance who have an Authorised Palliative Care and End-of-Life Care Plan in place do not need to be transported to the ED?
Ambulance authorised care plans can help you and your patients prepare for traumatic events before they occur. Recognising that some people in the community will require ambulance services several times, NSW Ambulance has developed a set of care plans to help them make the best decisions about your patients in the event of an emergency.
All Authorised Care Plans are completed by the GP and patient. These plans are submitted to Ambulance NSW, with a copy given to the patient, and need to be reviewed annually.
CLICK HERE for the Authorised Adult Palliative Care Plan instruction sheet.
CLICK HERE for the Authorised Care Plan fact sheet.
Memory Problems? – A new resource for people with dementia and their carers!
An informative guide has been produced by the Northern Sydney Dementia Partnership, a collaboration between Northern Sydney Local Health District, Sydney North Health Network, Alzheimer’s Australia and CCNB Northern Sydney Regional Dementia Planner.
The brochure provides succinct and relevant information for health professionals, people with dementia and their carers. We encourage your practice to display the Memory Problems Brochure in your practice and have it available for patients and families who would benefit from this important information.
The brochure provides information on education including the stages of dementia and what to expect, local support groups, service to help at home for both person with dementia and their carer, financial advice, legal matters, planning for the future and palliative care services.
If your practice subscribes to InfoMed the brochures will be delivered automatically. SNHN will also provide each practice with 50 brochures and a reorder form. If you would like more information regarding the supply of brochures, please contact the Primary Care Advancement team e: PCAIT@snhn.org.au
CLICK HERE for the Memory Problems brochure

New Lung Foundation Australia Lung Cancer Resources for Patients and Health Professionals
Lung Foundation Australia has recently developed two new lung cancer resources for patients and health professionals.
Lung Cancer Multidisciplinary Team Directory
The MDT Directory is a first for clinicians, patients and consumers. It facilitates referrals to hospitals delivering MDT-based lung cancer management, improving access and treatment for patients who present to their GP or clinician with symptoms of lung cancer.
The MDT Directory is an online tool that facilitates referrals to hospitals delivering MDT-based lung cancer management, improving access and treatment for patients who present to their GP or clinician with symptoms of lung cancer.
CLICK HERE to view the directory. For more information email Claire Mulvihill, Lung Cancer Support Nurse, at lungmdt@lungfoundation.com.au or freecall 1800 654 301.
Your Pathway Through Lung Cancer Care
Your Pathway Through Lung Cancer Care (LCCP) is a resource for patients that shows them what to expect following a diagnosis of lung cancer. It helps them understand more about lung cancer and the evidence-based pathways throughout their lung cancer journey, represented as ‘stepping stones’.
The LCPP aims to improve outcomes for lung cancer patients by empowering them and their families with clear information about their diagnosis and what to expect as a result of their diagnosis so that they can be active participants in their treatment. It will facilitate dialogue with health professionals.
CLICK HERE to view the LCCP which also links to the Lung Foundation’s ‘Better Living with Lung Cancer’ resource.
For more information or for a printed copy contact Lung Foundation Australia on freecall 1800 654 301 or e: enquiries@lungfoundation.com.au.

Treating and managing dysphagia and how to refer to a Speech Pathologist
Did you know we swallow over 900 times a day? Swallowing is a complex action involving more than 50 muscles and 6 cranial nerves. Swallowing involves an oral, pharyngeal and oesophageal phase.
Speech Pathologists assess, diagnose and treat people with oral and pharyngeal dysphagia. Dysphagia can occur following stroke, neurodegenerative diseases, head and neck cancers, radiation therapy, ageing or deconditioning.
Signs of dysphagia can include coughing after eating or drinking, choking, wet/gurgly voice after meals, sensation of food getting ‘stuck’ in the throat, weight loss, recurrent chest infections, difficulty managing secretions, or food and drink spilling out of the mouth. Dysphagia can significantly affect a person’s quality of life.
Speech Pathologists assess a person’s oral musculature and swallow with different food and drink consistencies and conduct objective assessments to visualise anatomical structures and swallow physiology. Objective assessments include:
- Videofluoroscopy (modified barium swallow), a video x-ray of swallowing
- Fibreoptic Endoscopic Evaluation of Swallowing (FEES), a scope is passed to view the larynx and pharynx while swallowing.
Following a comprehensive swallow assessment, Speech Pathologists treat the physiological abnormality of swallowing through prescribing swallowing exercises, compensatory strategies or diet modification. Speech Pathologists do not manage oesophageal dysphagia. Please consider gastroenterology input for these cases.
The NHSLD provide free services for patients with dysphagia, including:
- Outpatient clinical assessments
- Outpatient objective assessments
How to refer to Speech Pathology (adult services):
- Hornsby Hospital: Call 9477 9554 or fax a referral to 9477 9262
- Northern Beaches Health Service: Call 9998 0765 or fax a referral to 9998 0334
- Royal North Shore Hospital: Fax a referral to 9463 1067.
- Royal Rehab: Call 98089218 or fax a referral to 9807 3267
- Ryde Hospital: Call 9858 7812
Source: Alyssa Gearin, Speech Pathologist.

Revision of the healthy blood pressure guidelines
A revision of the healthy blood pressure guidelines for Australians has been released by the Heart Foundation. The new guidelines take a more holistic approach to blood pressure and are based on assessments of ‘absolute risk’. The guidelines encourage general practice to look at a composite of factors including blood pressure, cholesterol and diabetes.
The main changes are found in managing high risk groups and are relatively minor. The Heart Foundation, however, wanted to ensure the guidelines were aligned to the latest evidence and best practice.
CLICK HERE to read the new guidelines.

Making innovative use of cohort data to inform health service delivery
The third issue of Public Health Research & Practice for 2016 is now available, with the issue focusing on the innovative use of cohort data to address emerging public health issues and help inform the way health services are delivered on the ground.
Public Health Research & Practice (PHRP) is Australia’s first online-only open access peer-reviewed public health journal, published by the Sax Institute, with a strong focus on the connection between research, policy and practice.
The potential for Sax Institute’s 45 and Up Study – a longitudinal study of healthy ageing involving a cohort of more than 250,000 people in NSW ‒ to inform health services policy and planning is the focus of a perspective in the journal. The article describes how the Study data can be used to improve integration and coordination of services in Sydney, as well as how such data could be useful in supporting the work of Local Health Districts and Primary Health Networks (PHNs) throughout NSW.
Another paper describes how the Study of Environment on Aboriginal Resilience and Child Health (SEARCH) has developed into a long-term platform for closing the gap.
And finally, two research papers suggest that hospital emergency departments and intensive care units are prime settings for improving public health. One paper confirms smoking is more prevalent among patients in emergency departments than in the general population; the other describes how NSW has the opportunity to establish public health surveillance within intensive care units, which can help to protect the population from dangerous pathogens.
CLICK HERE to subscribe to e-alerts when the journal is published.
Source: The Sax Institute
[contentblock id=1 img=gcb.png]
