GP News – Oct ’16
Contents
- SNPHN commissions services for social work and dementia
- Redesigning the Practice Incentives Program – Important consultation process currently being undertaken by the Australian Government Department of Health
- Quality Improvement and PDSAs
- Temporary Amendment for ePIP
- Shared Antenatal Care GPs – updating details on the SNPHN website
- The National Shingles Vaccination Program
- Advance Project – new education opportunity for practice nurses
- Australian Asthma Handbook
- General Practice in-service briefings on community care
- GPs caught out by increase in female requests for genital cosmetic surgery: study finds
- Indigenous eye health program
- University of Sydney want to know your thoughts on antibiotics and resistance

SNPHN commissions services for social work and dementia
GPs are reminded that two newly commissioned services: Social Work Service to Support GPs is available for suitable patient referral by a GP, while The Hospital Discharge Follow Up Service for People with Dementia (hospital to home) is a hospital referred service to support your patients being discharged home safely. These local services have been designed to reduce the likelihood of admission or re-admission to hospital. Read about the individual services and how to refer below.
GP Social Work Support Program – Primary and Community Care Services (PCCS)
The funding provided to PCCS will allow the organisation to run a GP Social Work Support Program in Hornsby, Ku-ring-gai, Ryde and Hunters Hill, which adopts a patient-centred medical home approach to supporting the health, social and welfare needs of patients. The model works alongside a GP’s normal model of care, and provides social work services in the community to assist patients to improve their health and wellbeing, better navigate the system, access needed support, and avoid unnecessary hospitalisations. Social workers will support GPs and their patients by facilitating and coordinating additional assistance, for example liaising with social, welfare and community providers.
CLICK HERE for the PCCS GP Social Work Connect Flyer
CLICK HERE for the PCCS GP Social Work Connect Referral Form
Social Worker GP Support – Community Care Northern Beaches (CCNB)
Access to timely and effective social work services is key to helping people stay Healthy at Home. CCNB will deliver this model through the provisions of a mobile team of experienced and qualified social workers who will work flexibly across the LGAs of Willoughby, Lane Cove, Mosman, North Sydney, Manly, Warringah and Pittwater.
CLICK HERE for the CCNB Referral Form
CLICK HERE for the CCNB Flyer for GPs
CLICK HERE for the CCNB Social Work Medical Direction Template (right-click and “Save as…”)
CLICK HERE for the SNPHN instructions on importing templates into Medical Director.
CLICK HERE for the CCNB Social Work Best Practice Template (right-click and “Save as…”)
CLICK HERE for the SNPHN instructions on importing templates into Best Practice.
Dementia hospital discharge pilot project – KinCare
Kincare is an organisation that provides in-home health and wellbeing services to older people and people with a disability. SNPHN is commissioning Remember Me, a dementia-specific hospital discharge pilot project. The primary goal of the project is to facilitate the smooth transition of a person living with dementia from hospital to home. It also aims to reduce re-admissions to hospital, and to ensure all parties in the client’s support network are kept up-to-date through maintaining and improving communication. KinCare’s services are person-centred, flexible and responsive to changing needs.
CLICK HERE for the KinCare referral form
CLICK HERE for the KinCare Remember Me Brochure
Stay at home hospital discharge pilot project – Just Better Care (JBC)
JBC is one of Australia’s leading supplier of in-home support, enabling people to live independently, maintain their personal and social connections and enjoy a better quality of life. Stay at Home is a hospital discharge pilot project for people with dementia or suspected dementia who are being discharged from hospital and are at risk of re-admission. The project will provide participants with assistance through case management to link into services, supporting them to live as independently as possible in their own homes. A key component of the service is to ensure the patient’s GP is kept well informed of the discharge plan.
CLICK HERE for Stay at Home brochure
CLICK HERE for Stay at Home poster
For more information, please contact the Primary Care Team.
T (02) 9432 8250 F (02) 8088 4770
e: pcait@snhn.org.au
Mon – Fri, 9:00am – 5:00pm

Redesigning the Practice Incentives Program – Important consultation process currently being undertaken by the Australian Government Department of Health
The Practice Incentives Program (PIP) is a key driver of quality care in the general practice sector. The redesign of the PIP is an Australian Government initiative to simplify the current PIP and to introduce a new Quality Improvement Incentive. This will give general practices increased flexibility to improve their detection and management of a range of chronic conditions, and to focus on issues specific to their practice population.
The Department of Health is now seeking stakeholder views on how the PIP might foster quality improvement and innovation and offers a number of ways that stakeholders can participate in the consultation. Opportunities include:
- Indicating your interest in participation through a forum or webcast at the Department of Health online consultation hub at consultations.health.gov.au
- Providing a written submission that comments on specific elements or all elements of the Consultation Paper – Redesigning the Practice Incentives Program
- Responding to the anonymous questionnaire that will be available at consultations.health.gov.au
We look forward to receiving your valuable input to this important consultation process to ensure your views contribute to the innovative and collaborative redesign of the PIP in the support of quality health care.
Quality Improvement and PDSAs
If you are interested in Quality Improvement and have the CATPlus Tool installed at your practice, SNPHN will provide you with a payment of up to $1000.00 if five Plan Do Study Acts (PDSAs) are completed by 30 June 2017 – this equates to $200.00 per completed PDSA.
If you do not have CATPlus installed and would like to participate in quality improvement, we can arrange to have the tool installed.
For more information, please contact the Primary Care Team.
T (02) 9432 8250 F (02) 8088 4770
e: pcait@snhn.org.au
Mon – Fri, 9:00am – 5:00pm

Temporary Amendment for ePIP
A temporary amendment to the ePIP incentive has been made by the Department of Health to allow general practices participating in the program to upload all shared health summaries required to meet targets to the My Health Record by January 31 2017.
For practices that opted out in the first quarter, they will now have the opportunity to catch up and meet their shared health summary targets so they can receive the full incentive.
For practices that do not intend to meet all ePIP requirements, the Department suggests they should withdraw from the program. This will ensure practices are not overpaid, and not faced with having to repay up to three quarterly payments.
The Department will formally communicate this arrangement to ePIP registered practices over the coming weeks.
For more information, please contact the Primary Care Team.
T (02) 9432 8250 F (02) 8088 4770
e: pcait@snhn.org.au
Mon – Fri, 9:00am – 5:00pm

Shared Antenatal Care GPs – updating details on the SNPHN website
If you’re a SAC GP, you were recently asked to complete an updated details and consent form for your information to be made public on the SNPHN website. GPs who did not return this form were removed from the publicly available shared antenatal care list. You can check this by visiting the SAC webpage and pressing ‘CLICK HERE to find a SAC GP’. If you would like to be reinstated on the list, please download the details form and return to SNPHN at your earliest convenience.

The National Shingles Vaccination Program
The National Shingles Vaccination Program will commence from 1 November 2016.
People eligible to receive the free shingles vaccine include:
- People aged 70 years of age as an ongoing program.
- People aged 71-79 years of age as a catch-up program until 31 October 2021.
People who are not eligible to receive the vaccine as part of the program can purchase the vaccine on the private market.
Providers should submit shingles vaccination data to the Australian Immunisation Register (AIR), which commenced in September 2016, expanding upon the Australian Childhood Immunisation Register (ACIR) by capturing vaccines administered throughout a person’s life.
- Fact Sheet for vaccination providers, providing information on eligibility; co administration of the shingles vaccines with other vaccines; and how to report adverse events
- Brochure for consumers, including frequently asked questions
- Poster promoting the vaccine
- Poster promoting the vaccine – Aboriginal and Torres Strait Islander people
- Fact Sheet for vaccination providers regarding the newly expanded Australia Immunisation Register (AIR)
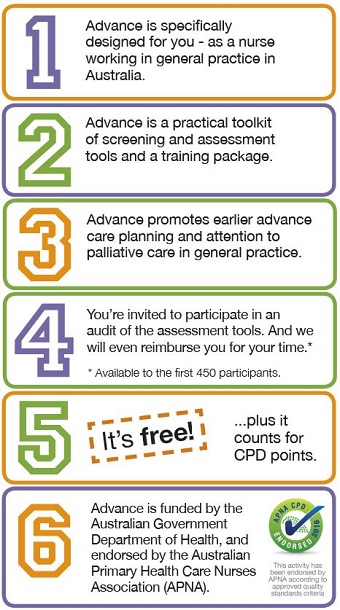
Advance Project – new education opportunity for practice nurses
What is Advance?
Advance is a free toolkit of screening and assessment tools and a training package, specifically designed to support nurses in Australian general practices to work with general practitioners (GPs) to initiate advance care planning (ACP) and palliative care in everyday general practice.
The Advance Toolkit consists of six screening and assessment tools and a Guide, which indicates how to implement the screening tools in a systematic way in general practice. The toolkit was informed by a literature review of the best available evidence about tools to support palliative care and ACP in general practice, as well as input from our expert advisory group and feedback from general practice nurses, general practitioners and Carers Australia.
Who is it for?
Only registered and enrolled nurses who are currently working in Australian general practice are eligible.
What is the aim of Advance?
Advance aims to enable better care outcomes in Australian GP practices through:
- enabling earlier consideration and uptake of ACP enabling more efficient use of GP and nurse time in providing palliative and supportive care
- enabling more appropriate and timely referrals to specialist palliative care services if required
- increasing confidence and comfort levels for general practice nurses (GPNs) in initiating conversations with patients and their carers about screening for supportive care needs and ACP.
Why nurses in general practices?
General practices provide ongoing care for a large number of patients with chronic, debilitating and eventually fatal diseases, both malignant and non-malignant conditions. Thus general practices have an essential role in providing palliative care to patients and their families. GPNs play a key role in patient management within general practices. GPNs are already involved in managing patients who are at risk of deteriorating health and dying. Given their ongoing relationship with patients and carers and the level of trust developed, GPNs may be ideally placed to help such patients identify their most important symptoms, concerns and priorities that they would like addressed by their GP.
What are the benefits of Advance for general practice?
The Advance training package will help general practice nurses to work with GPs to initiate ACP and, where appropriate, palliative care for elderly and/or chronically ill patients within the practice. This will:
- Help break down some of the barriers to ACP in general practice
- Enable the practice to more efficiently:
- identify patients who might be at risk of deteriorating and dying
- assess and address the supportive care needs of patients who might be at risk of deteriorating and dying
- assess and address the needs of carers of patients who might be at risk of deteriorating and dying
- Help identify patients who might benefit from early referral to specialist palliative care services.
How is the training funded and delivered?
The program is available free of charge for nurses working in Australian general practice. Advance is funded by the Australian Government Department of Health and will be delivered by a national consortium. There is free online training, free face-to-face workshops, free one-to-one tele-mentoring from an experienced palliative care nurse, sponsorship for completing patient assessments, and more. The training will count towards your GPN’s CPD requirements.
How much time will it take a general practice nurse to complete the training and where will the training be delivered?
The online component of the training package will take about two hours in total to complete. The free practical workshops will be held on weekday evenings in every capital city of Australia for approximately 3 hours. Scholarships will be made available for GPNs from rural/remote settings to assist with their costs to attend the workshops.
You can find out more about Advance here.
Free Advance practical workshop on 27 October
A practical workshop is being held on Thursday 27 October at Ku-ring-gai Gordon library for nurses working in General Practice. The workshop is on “Initiating palliative care and advance care planning”.
CLICK HERE for more information.

Australian Asthma Handbook
The National Asthma Council Australia launched version 1.2 of the Australian Asthma Handbook, developed by an interdisciplinary team of medical experts and incorporating feedback from primary care providers. Implementation of treatment plans for asthma will get easier for GPs, with the updated Handbook clarifying facts on the latest medications on the market for asthma and chronic obstructive pulmonary disease (COPD).
CLICK HERE to access the online handbook.
CLICK HERE for the media release.

General Practice in-service briefings on community care
Not for profit community care service CCNB works closely with a range of health professionals on supporting the continuity of care for their patients. CCNB is an independent service providing impartial advice and free in-service briefings to general practices on a range of social care topics, such as:
- GP social worker service
- Changes to Australia’s aged care system
- Roll out of National Disability Insurance Scheme
- Hoarding and squalor support services
- Dementia support services
If you would like an in-service presentation to your practice, please contact CCNB by email at ccnb@ccnb.com.au or by telephone on 1300 002 262.

GPs caught out by increase in female requests for genital cosmetic surgery: study finds
One-third of patients requesting female genital cosmetic surgery (FGCS) are younger than 18, according to a joint Monash study of Australian General Practitioners, with many GPs feeling ill-equipped to advise on the surgery.
Conducted by Monash University and the University of Melbourne, the study provides an insight into GP’s knowledge, attitudes and practice in managing patients who asked about the surgery.
The survey of 443 GPs found 97 per cent had been asked about genital ‘normality’, reflecting anxiety about this, and that more than half had seen patients requesting FGCS, ranging in age from as young as 10 years to 65 years.
Monash University’s Dr Jason Ong, who is a GP and sexual health physician, said advertisements and social media were promoting the procedures as “vaginal rejuvenation,” “designer vaginas” and “Barbie-plasty.”
“The thing that concerns me as a doctor is that a lot of these procedures are not proven as to their benefits and there are no studies about the long-term effects of having them.
“It’s important that GPs, as the first point of contact for many Australian women, are able to advise and reassure women about their genitalia,” Dr Ong said.
The popularity of FGCS is growing, mirroring trends in Britain and the US. Australian Government statistics indicate a 140 per cent increase in requests for rebatable vulvoplasty, from 640 in 2001 to more than 1500 in 2013, without a concomitant rise in genital disease diagnoses. Medicare has since reviewed the rebate for FGCS and now requires proof of a medical reason for the procedure.
Significantly, nearly half the GPs surveyed reported they had insufficient knowledge of the risks of FGCS procedures, suggesting they required greater education to support patients.
Melbourne University researcher and GP, Dr Magdalena Simonis, said: “They all felt it was a new phenomenon and felt unprepared for it.”
In the survey, GPs reported they believed their patients were influenced by fashion (appearance in clothes), comfort in clothes, perceptions of beauty and pornography, and peer group pressure. ‘Brazilians’ – women removing their pubic hair – had meant that genitalia were more visible to women and their partners.
However, more than half the GPs suspected that mental health difficulties such as depression, anxiety, relationship difficulties, partner abuse and body dysmorphic disorder in women were driving the requests for advice for FGCS.
The RACGP has produced the RACGP female genital cosmetic surgery guide for general practitioners and health professionals, which is free to download from the RACGP guidelines website .
Source: Monash University

Indigenous eye health program
Please see below for some information of new MBS Item numbers to help improve eye health for Aboriginal and Torres Strait Islanders, commencing 1 November 2016.
CLICK HERE for MBS Item numbers.
CLICK HERE for Budget information.

University of Sydney want to know your thoughts on antibiotics and resistance
Researchers at the University of Sydney invite general practitioners to participate in an Australian-wide survey on antibiotic use and resistance. The aim of the survey is to explore practitioners’ attitudes towards antibiotic use and resistance, education and resource needs. The survey takes about 15-20 minutes. All participants in the survey will have a chance to win an iPad.
CLICK HERE to participate in the survey.
Responses are anonymous and confidential. Your views are important to this study.
For more information, contact dale.dominey-howes@sydney.edu.au or call +61 2 9351 6641.
[contentblock id=1 img=gcb.png]
